What are varicose veins?
Varicose veins are swollen and twisted veins that develop when the small valves inside the veins stop working properly. Normally, these valves help blood flow smoothly back to the heart and prevent it from flowing backwards. If the valves become weak or damaged, blood can pool in the vein, making it swollen and twisted.
While many people worry about how they look, varicose veins are actually a medical condition known as varicose vein disease. They can sometimes cause pain or lead to more serious health problems if not treated in a timely manner.

"A popular misconception is that varicose veins are cosmetic. They signify a poorly functioning circulation and often progress over time. Treatment of varicose veins in a timely fashion ensures optimal vein health and minimises the risk of medical complications from poorly functioning veins."
Mr Ed Sideso
Consultant Vascular Surgeon, UK Vein Clinic and Vascular Lead at John Radcliffe Hospital Trust
How varicose veins develop
Several factors increase the risk of developing varicose veins:
- Family history: If others in your family have them, you’re more likely to get them too.
- Age: Veins get weaker as you get older.
- Pregnancy: Increases blood flow and pressure on your leg veins.
- Being overweight: Puts extra pressure on your veins.
- Standing or sitting for long periods: Makes it harder for blood to flow upwards.
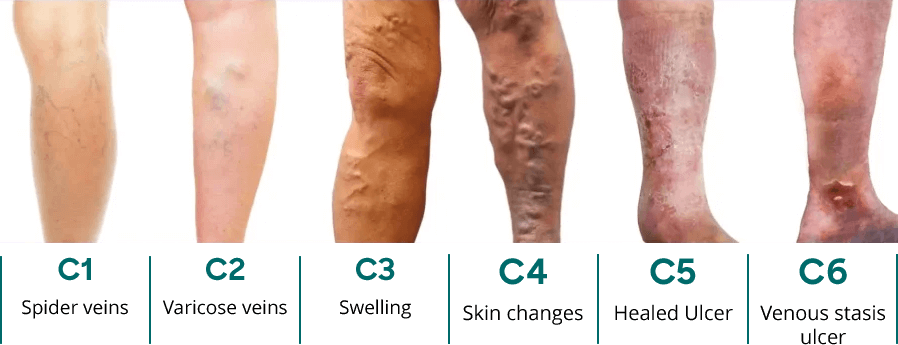
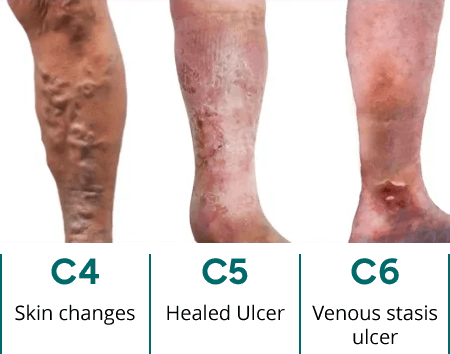
One of the standardised ways that varicose veins are categorised is using a classification guide called the CEAP score. As you can see in the diagram below, vein disease has a number of stages which highlights that it is a progressive disease.
This score also helps doctors to classify the severity of a patient’s varicose veins or vein disease and help guide treatment decisions.

Who is affected?
Varicose veins can affect anyone, but certain factors increase the risk.
Age plays a significant role in who might develop varicose veins. According to the National Institute of Health and Care Excellence (NICE), around 41% of all varicose vein patients are above 60 years old. However, it can also impact younger age groups too.
This is because as you age, veins can lose elasticity, causing them to stretch and the valves in your veins become weak. This weakening then allows blood that should be moving towards your heart to flow backward. This blood pools in the veins, causing them to enlarge.
Other than age, genetics can also be an indicator for who might be affected. If members of your family have varicose veins, this might mean that you’re more susceptible too. Studies have shown that if one parent has varicose veins, the risk for the child (in adulthood) is about 40% but can increase to 90% if both parents have varicose veins.
Studies also show that women are more likely to be affected than men. This is because hormone changes through pregnancy, around periods or during menopause can make vein walls weaker.
Varicose vein symptoms and clinical features
Spotting the symptoms early can help you manage and treat varicose veins more easily and stop them from getting worse.
Common signs and symptoms
Visible veins
One of the main signs of varicose veins is being able to see them on your skin. These veins usually look blue or dark purple and are often twisted and bulging, like cords or ropes.

Aching, heavy, or tired legs
Varicose veins can cause aching, heaviness, or discomfort in your legs. This discomfort may worsen after standing or sitting for long periods. Some individuals also experience throbbing or burning sensations. Some studies have shown that over 55% of patients with varicose veins will also experience itching or aching legs.
Swelling/oedema in the ankles & feet
Swelling in the lower legs and ankles is another common symptom. You might also experience muscle cramps, particularly at night.
Burning, throbbing or cramping sensation
A burning, throbbing, or cramping feeling in your legs can happen with varicose veins, and these symptoms often get worse after standing or sitting for a long time.
Itching or skin irritation around the veins
Itching or skin irritation around the veins can be a result of inflammation and poor circulation caused by varicose veins. This often affects the lower legs and may be an early sign of skin changes, such as dryness, flaking, or even eczema in more advanced cases.
Restless legs, especially at night
At night, when you move less and blood flow slows down, pressure can build up in your legs. This can make your legs feel restless and give you a strong urge to keep moving them, which is common in people with varicose veins.
Complications
Symptoms of varicose veins often worsen after long periods of standing or sitting, during hot weather, or after strenuous activity. Many people find their discomfort increases as the day progresses, and symptoms may be particularly noticeable in the evening. Below are some of the examples of more advanced symptoms.
Leg ulcers
When blood doesn’t flow well in the legs, the skin can get damaged over time. This can lead to painful sores called venous ulcers, which heal very slowly. These sores happen because poor blood flow puts extra pressure on the veins and skin, making it harder for wounds to get better.
Here's how this happens, step by step:
- Valve failure in leg veins: In healthy veins, tiny one-way valves help blood flow upwards towards the heart. When these valves become weak or damaged, they stop working properly.
- Blood pooling: Instead of flowing as it should, blood begins to collect in the lower part of the leg. This builds up pressure inside the veins, particularly around the ankles.
- Increased pressure and fluid leakage: The higher pressure in the veins forces fluid and blood cells out into nearby tissues. This can cause swelling, inflammation, and skin changes like dryness or discolouration.
- Skin breakdown: Without enough oxygen and nutrients reaching the skin—due to poor circulation—the skin becomes fragile. Over time, it can start to break down.
- Ulcer formation: Eventually, a sore or ulcer forms. This is often shallow but painful and can take a long time to heal. It usually appears on the inner side of the lower leg or ankle and is more likely to become infected if not treated promptly.
If you notice any signs of skin changes or sores on your lower legs, it’s important to speak to a healthcare professional. Early treatment can prevent ulcers from becoming more serious and help improve healing.
Skin discolouration
When varicose veins go untreated, they can cause changes in the skin, especially around the ankles. One common change is the skin becoming darker—often a reddish-brown or purplish colour. This happens because the valves in your leg veins stop working properly, allowing blood to pool and pressure to build up.
Over time, the increased pressure pushes red blood cells out of the veins and into the surrounding tissue. When these cells break down, they release iron, which gets stored in the skin. This iron causes the skin to darken, a condition called haemosiderin staining.
You may also notice the skin becoming thin, dry, itchy, or more fragile. These changes are signs of long-standing vein problems and indicate one of the more advanced stages of vein disease. If left untreated, the skin can eventually break down, leading to ulcers.
Getting help early can prevent further damage and improve skin health. If you notice skin darkening or irritation near your ankles, it’s worth speaking to a healthcare professional.
Thrombophlebitis
Thrombophlebitis is when a varicose vein becomes inflamed due to a small blood clot forming just under the skin. It often happens because blood isn’t flowing properly through damaged veins, making it easier for clots to develop. This can cause:
- Redness and swelling along the vein
- A firm, tender area that may feel warm
- A raised, rope-like vein under the skin
This condition is called superficial thrombophlebitis because it affects veins near the surface. It’s usually not serious but can be painful. Treatment often includes warm compresses, leg elevation, and compression stockings.
If you notice these symptoms, it’s important to get checked, especially to rule out deeper vein problems.
When symptoms may worsen
Varicose veins are a progressive condition, which means symptoms can gradually get worse over time if left untreated.
In the early stages, you may only notice mild aching or visible veins, but over weeks or months, symptoms can become more frequent or intense. For many people, discomfort—such as heaviness, swelling, or cramping—builds as the day goes on, becoming most noticeable in the evening.
As the condition progresses, you might start to see new symptoms like itching, skin changes, or restless legs. These signs suggest that the vein problem is getting worse and that blood flow in the legs is becoming more affected.
It’s important to recognise that worsening symptoms aren’t just a sign of discomfort—they’re an indication that your veins are under increasing strain. Getting assessed early can help prevent more serious complications, like skin damage or ulcers, from developing later on.
Can varicose veins hurt?
Many patients wonder, "Should varicose veins be painful?" The answer is yes, you can experience painful varicose veins, especially as the condition progresses. The pain may feel like aching, burning, or cramping, particularly after long periods of standing or at the end of the day.
What causes varicose veins?
As outlined above, the main causes of varicose veins are faulty valves within the veins that cause blood to flow backward and pool. This, over time, can lead to the faulty veins being bulgy, achy, itchy or make your legs feel really heavy.
Risk factors you should know
For some people, the development of varicose veins might be due to the presence of one or more of the following risk factors:
Family history of varicose veins
Whilst not always a guarantee, genetics can play a really big role in whether someone might develop varicose veins. If your parents or relatives have experienced varicose veins, you are at a higher risk for also developing them.
Gender
Women are more likely to develop varicose veins than men due to the changes to hormone levels that women experience. Changes to the body during pregnancy or menopause, for example can increase the risk for women.
Excess weight
Carrying extra body weight puts more pressure on your veins. This extra pressure can make the tiny valves inside your veins weaker over time, making it harder for blood to move up toward your heart. This disrupts normal blood flow, which in particular can lead to varicose veins in legs and feet.
Lack of physical activity
Lack of movement throughout the day or sitting for long periods of time can increase the risk of varicose veins. This is because blood is not being pumped around your body.
Occupation type
Certain jobs which require you to be standing or sitting for long periods of time can increase the overall risk of developing varicose veins. Office based jobs or jobs in fields like healthcare means that you’re more likely to develop varicose veins.
How varicose veins are diagnosed
If you think you have varicose veins, it’s important to get a proper diagnosis. This helps your healthcare provider understand how severe the problem is and decide on the best treatment for you. Diagnosis is straightforward and usually involves a physical examination and a painless scan.
Diagnostic tests (e.g., duplex ultrasound)
A duplex ultrasound scan is the gold standard for diagnosing varicose veins. This painless, non-invasive test uses sound waves to create images of your veins and check blood flow, helping to see the exact location and cause of valve failure. This scan should be carried out by a Vascular Scientist using a Doppler ultrasound machine to accurately map out veins that require treatment.
This scan usually starts right at the top of your thigh near your groin, to assess for deeper vein issues (if present). This mapping allows the Vascular Scientist and Vascular Doctor to develop a detailed diagnosis which forms the basis of your personalised treatment plan.

Clinical examination
Following the scan, a vascular doctor will take the time to take you through the results of your scan, and their recommendation for treatment.
This part of your appointment is an opportunity for the doctor to also discuss medical history, your experience with varicose veins and to perform a physical examination of your legs.
You'll also be taken through what to expect during your treatment, any risks but it also gives you a chance to ask any questions that you might have.
Treatment options for varicose veins
If you have varicose veins, there are several treatment options available depending on your symptoms and how severe your veins are. Below you’ll find a few of the more management techniques through to the more proactive treatment options.
Conservative management (lifestyle changes, compression stockings)
Regular exercise
Doing regular exercise is very important if you have varicose veins. Activities like walking, riding a bike, or swimming help your blood move better in your legs. This takes some pressure off your veins. Aim for at least 30 minutes of exercise most days.

Healthy diet
Eating a balanced diet with lots of fibre and low salt can help reduce symptoms such as swelling. Eating a well-rounded diet can help you maintain a healthy weight and reduce the stress on your circulation.
Elevation
During the day, try to take breaks to lift your legs up above your heart. This can help lower swelling and help your blood flow better.
Compression stockings
For the best results, wear your compression stockings throughout the day. They are typically most effective when put on in the morning before swelling occurs.

Minimally invasive treatments
Whilst lifestyle changes are the best place to start, some people find that this isn’t enough to significantly improve their varicose veins. The good news is that there are minimally invasive treatments available to help you get back to feeling your best.
Endovenous radiofrequency ablation (EVRF)
EVRF, also called radiofrequency ablation (RFA), is a modern way to treat varicose veins. In this treatment, a doctor puts a thin tube(called a catheter) into the vein. Then, they use radio waves to heat up the vein causing it to close up. Over time, your body absorbs the closed vein, rerouting your blood to healthier veins.
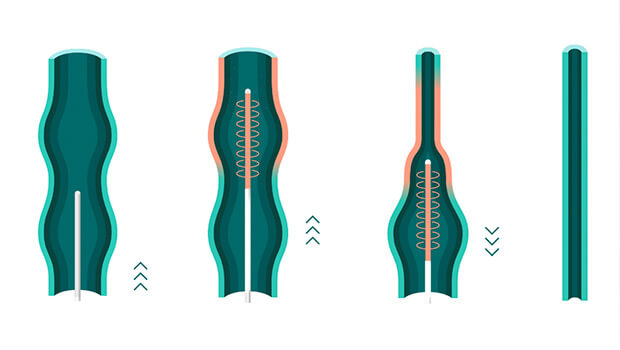
RFA is often the first treatment doctors use for varicose veins. It is done with a local anaesthetic, so only the area being treated is numbed. Most people say the treatment does not hurt much, but everyone feels pain differently. Nurses help patients feel calm and distracted during the treatment, which can make it feel less painful. This is called verbal anaesthesia and works very well for many people.
RFA works best when the veins in the thigh are straight. This makes it easier for the doctor to put the catheter in and heat the vein from the top of the thigh down. After this treatment, blood flows better, and the veins you can see on the surface of your skin often fade over time.
As this is a minimally invasive treatment, there is minimal downtime meaning you can get back to your routine within a day or two.
A recent study of 3,455 patients showed that 79% of UK Vein Clinic patients had RFA as their main treatment. Although RFA is one of the main ways to treat varicose veins, it can sometimes also be used together with foam sclerotherapy (see below).
Foam sclerotherapy
Foam sclerotherapy is a treatment that involves injecting a harmless foam solution into the varicose vein. This solution blocks off blood flow in these veins, causing it to seal off and collapse over time so that the body can naturally absorb it into the body.
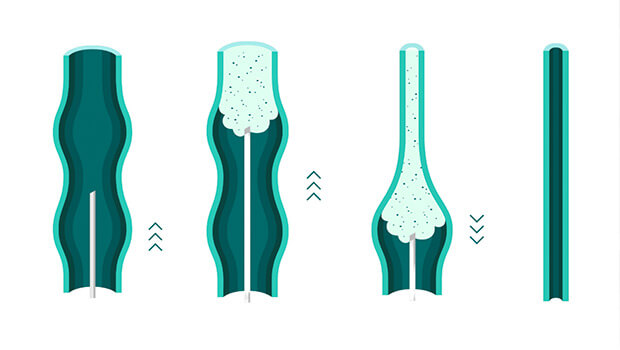
It is typically a second line treatment used for treating some of the more bulging and wiggly veins on the lower half of limbs that can't be accessed using the RFA catheter. It's proven highly successful for effectively closing down these types of varicose veins and can also be used to tidy up some of the smaller veins on the surface of your skin to achieve a more optimal cosmetic outcome.
As this is a minimally invasive treatment, there is minimal downtime meaning you can get back to your routine within a day or two.
The results of RFA and foam sclerotherapy are enhanced when the diagnostic scan and clinical examination are performed by expert vascular scientists and vascular doctors.
Surgical options (if applicable)
Vein stripping
Vein stripping is a traditional surgical method done under general anaesthetic to treat varicose veins. During this surgery, the surgeon will first make a small cut near the groin and tie off the vein to prevent blood flow. A similar step is done lower down on the leg, where the surgeon can then gently pull the vein through the cut.
This surgery is more invasive and takes between 1-1.5 hours to complete with a recovery time of 2-4 weeks.
Vein stripping is not as commonly used because minimally invasive and highly effective treatment options such as RFA are now available. In most cases, vein stripping is an unnecessarily traumatic procedure and should only be considered when all other modern methods have been ruled out.
Phlebectomy (avulsions)
Phlebectomy, also called ambulatory phlebectomy, is a simple surgery to remove varicose veins that are close to the surface of your skin. In this treatment, the doctor makes a few tiny cuts along the vein. Then, the doctor uses a small hook to gently pull out the vein.
This is done under local anaesthetic, which means the area is numbed but you are awake. Most people can go back to their normal activities in just a few days.
Phlebectomy works well for very large varicose veins near the surface of your skin, particularly when there’s a higher risk of foam sclerotherapy causing skin staining.
In the same study of 3,455 patients at UK Vein Clinic, a phlebectomy was only required for less than 1% of all patients.
Minimising varicose vein risks
What are the risks of varicose vein treatment?
When you think about getting treatment for varicose veins, it’s good to know about possible side effects. Most side effects for minimally invasive procedures are mild and don’t last long, but knowing about them can help you feel ready.
New thread veins and matting
After treatment, especially after sclerotherapy, some people see new, tiny red or purple veins (called thread veins or spider veins) near where they were treated.
Sometimes, these veins form a web-like pattern called “matting.” This is usually not harmful, but some people don’t like how it looks.
Skin staining
Sometimes, the skin along the treated vein turns brown. This is called skin staining. It happens when some blood leaks into the skin.
It’s a common short-term risk associated with varicose vein treatment. Generally skin staining is mild in nature, localised to the vein and fades over time.
2cm in diameter or below with low contrast to a patients’ skin tone is considered mild staining.
Phlebitis (vein inflammation)
The treated vein can get sore, red, and feel hard under the skin. This is called phlebitis.
Phlebitis is pretty common after treatments like sclerotherapy. It usually goes away on its own or with things like wearing compression stockings or taking medicine for pain.
New varicose veins
Even after treatment, new varicose veins can appear later. This is because the cause (like weak vein valves) can still be there.
Some people may need more treatments in the future.
Treatment might not work fully
Sometimes, the treated veins don’t go away completely, or you might still have aching or swelling.
You might need more than one session or a different treatment to get the best results.
Deep Vein Thrombosis
Varicose vein treatments can increase the risk of deep vein thrombosis (DVT) because procedures may damage blood vessels or slow blood flow, leading to clot formation. Although the risk is generally low, it’s important to keep moving after treatment.
How to minimise the risks of treatment
To get the best results from your varicose vein treatment and lower the chance of problems, you can do these simple things:
Assessment with a vascular doctor
Why: Having a thorough assessment from a vascular doctor prior to treatment can help identify any potential risks or concerns.
How: Visit a clinic that can provide a thorough vascular and medical assessment before you proceed to treatment.
Wear compression stockings after treatment
Why: Compression stockings help reduce swelling, support healing, and improve circulation – especially important after treatment.
How: Wear them as advised by your healthcare provider-usually for at least one week during the day after your procedure.
Stay active
Why: Moving around helps your blood flow and lowers the risk of blood clots.
How: Take short walks often, and try not to stand still for too long, especially in the first few days after your treatment.
Follow aftercare instructions
Why: Proper aftercare is essential for recovery and minimising complications.
How: Avoid strenuous exercise or heavy lifting for a few days. Keep the treated area clean and dry as instructed.
Watch for signs of complications, such as increased redness, swelling, or severe discomfort, and contact your healthcare provider if these occur.
What to expect during and after varicose vein treatment
The process for getting your veins treated is usually quite straightforward and split into four key steps:
1

Diagnostic assessment with vascular scientist
2

Examination & history with vascular doctor
3

Vein treatment with vascular consultant
4

Follow up & discharge managed by aftercare team
Before your treatment
Before your treatment, you’ll have a comprehensive assessment, including a ultrasound scan and a discussion of your treatment options with vascular experts.
In preparation for your treatment, it's important to follow any guidance from your healthcare team. For example, wearing loose fitting clothing to your appointment so that you can easily pull these over your bandaged legs after treatment.
You may also want to bring a pair of loose shorts to wear during your procedure, this might make you feel more comfortable but also provides your vascular consultant with easy access during treatment. Alternatively, a disposable gown will usually be offered.
Prior to the treatment appointment, it's very common for patients to feel a little anxious about what to expect. Having treatment isn't an everyday occurrence but making sure you take the time to understand what happens during the appointment can help reduce some of these worries.
When you choose a reputable clinic for your procedure, you can be rest assured knowing you’re in the safe hands of experienced specialists.
During your procedure
During your treatment appointment, you'll be taken to a consultation room where a clinician will explain the procedure once more and get you to read and sign an informed consent form.
You'll then be asked to change into either a gown provided or loose shorts that you've brought with you. The team will get you settled down before they start your procedure. RFA and foam sclerotherapy are done under local anaesthetic and take less than an hour in total to complete - you'll be able to walk out of the clinic on the same day.
The clinical team (usually two nurses and a vascular surgeon) will keep chatting to you throughout your treatment. Once finished, you'll be bandaged up and compression stockings placed on top – you'll need to keep these on for the first 48 hours and make sure your small incisions remain dry.
Aftercare and recovery
After treatment, you may experience mild bruising, tightness, or tingling in your legs. These symptoms usually resolve within a few days.
You may be advised to take over the counter pain medication to help with any discomfort, but pain should mostly be tolerable.
You may be advised to wear compression stockings for a short period to support healing. Your healthcare provider should have an aftercare service available to help you once you’ve left the clinic – giving you peace of mind.
When to resume normal activities
Most patients can return to work, exercise, and normal activities within 24 to 48 hours. We recommend avoiding strenuous exercise or prolonged standing for a few days, but you can expect a quick return to your usual routine.
Follow-up appointments and long-term care
Follow-up appointments may be scheduled in the following months. These appointments allow your doctor to check progress and see how you’re healing.
An ultrasound scan may be repeated to check the successful closure of varicose veins and confirm that there are no complications.
Can varicose veins come back after treatment?
Varicose vein recurrence
Varicose veins can come back after treatment. This is known as recurrence which means that either the problematic vein has opened again, or that new veins (“de novo”) have become varicose following treatment.
This typically results from the natural progression of vein disease or in some cases incomplete treatment*. It’s important to get checked out by your healthcare team with a scan to get a better idea of the cause of varicose vein recurrence.
*A survey of 1118 patients who received treatment from UK Vein Clinic showed recurrence at 2.36% two years or more post treatment.
Preventing varicose veins
Lifestyle tips
Incorporating simple habits into your daily routine can make a difference. Elevating your legs when resting, avoiding prolonged periods of standing or sitting, and staying active are all beneficial practices.
Your doctor may also recommend dietary changes or supplements to support your vascular health. While not all varicose veins can be prevented, you can reduce your risk by:
- Staying active and exercising regularly
- Maintaining a healthy weight
- Avoiding long periods of standing or sitting
- Elevating your legs periodically
- Wearing compression stockings
- Add supplements such as vitamin E and C andomega-3 fatty acids into your diet
Early intervention
If you notice the early signs of varicose veins such as itching, aching or bulging veins, it’s best to get a doctor to take a look. Getting help early can help prevent the symptoms of varicose veins getting worse and can reduce the risk of complications.
When to seek medical advice
Signs you shouldn’t ignore
Varicose veins are not just a cosmetic concern – they can also lead to significant health issues if left untreated.
Knowing when to seek medical advice for varicose veins is crucial. Here are some signs you shouldn't ignore:
Persistent pain and swelling
If you have ongoing pain or swelling in your legs, it could be a sign of something more serious than just tired legs. If you notice constant aching, heaviness, or throbbing, it’s a good idea to talk to your doctor.
Skin changes and discolouration
If the skin around your varicose veins change colour, becomes brownish, or looks swollen, it could be a warning sign. These skin changes might mean your vein problem is getting worse or that you could develop a sore (ulcer) if it isn’t checked.
Bleeding or ulceration
Bleeding from varicose veins or getting a sore (ulcer) on your skin is a serious warning sign. Ulcers can be painful and often take a long time to heal, so they need quick medical attention.
Sudden onset of symptoms
A sudden increase in symptoms such as swelling, pain, or changes in the appearance of the veins should not be ignored. Such symptoms could suggest a blood clot, which requires urgent medical attention.
How UK Vein Clinic can help
At UK Vein Clinic, we offer expert assessments, and a full range of treatment options tailored to your needs. Our team of leading vascular consultants and specialist practitioners are dedicated to delivering world-class care, from your first appointment to your final follow-up.
Take our two-minute diagnostic test to see if you could benefit from varicose vein treatment and start your journey to healthier legs today.
Why choose UK Vein Clinic for varicose vein treatment?
Expertise you can trust
With years of experience and leadership in vascular medicine, our specialist team are here to provide the best possible care to help patients get back to looking and feeling their best.
With years of experience and expertise in vascular medicine, our accredited team are leaders in their field.
Patient centred care
UK Vein Clinic takes a patient first approach. Our team takes the time to listen, understand and answer any questions you have, so that you always feel supported.
Advanced treatment options
Our specialists use the latest, clinically proven techniques like radiofrequency ablation and foam sclerotherapy, which are minimally invasive and recommended by NICE guidelines.
These treatments mean less discomfort, quicker recovery, and excellent long-term results, so you can get back to your normal life sooner and with confidence in your care.
Doctors who treat this condition
Related
Duplex ultrasound assessment
Radiofrequency ablation
Foam sclerotherapy

References
- Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study https://pubmed.ncbi.nlm.nih.gov/10396491/ (Accessed on: 24 June 2025)
- Varicose veins treatment in England: population-based study of time trends and disparities related to demographic, ethnic, socioeconomic, and geographical factors https://pmc.ncbi.nlm.nih.gov/articles/PMC9260184/ (Accessed on: 24 June 2025)
- Varicose veins in the legs: the diagnosis and management of varicose veins https://www.nice.org.uk/guidance/cg168/documents/varicose-veins-final-scope2 (Accessed on: 24 June 2025)
- Varicose veins: What are the causes and risk factors? https://cks.nice.org.uk/topics/varicose-veins/background-information/causes-risk-factors/ (Accessed on: 24 June 2025)
- Diagnosis and management of varicose veins in the legs: summary of NICE guidance https://www.bmj.com/bmj/section-pdf/724779?path=%2Fbmj%2F347%2F7918%2FPractice.full.pdf (Accessed on: 24 June 2025)
- https://www.nhs.uk/conditions/phlebitis/ (Accessed on: 24 June 2025)
- https://www.nhs.uk/conditions/leg-ulcer/symptoms/ (Accessed on: 24 June 2025)
- https://researchonline.lshtm.ac.uk/id/eprint/16938/ (Accessed on: 24 June 2025)

