What is Chronic Venous Insufficiency?
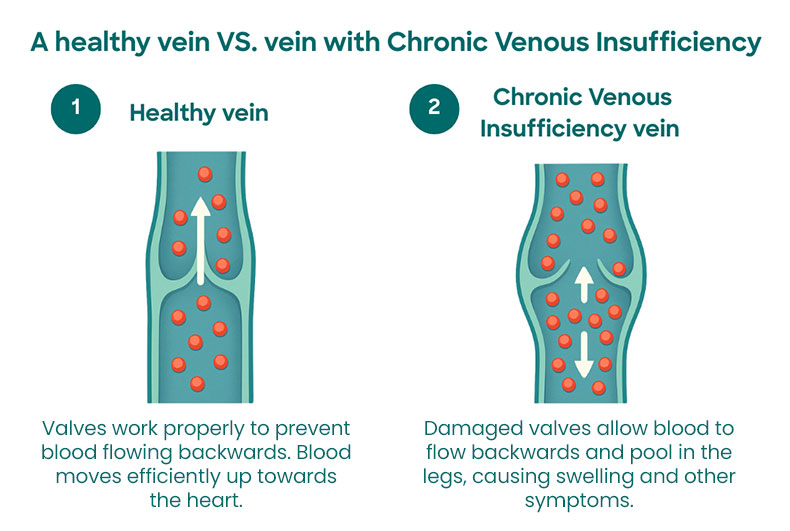
Chronic Venous Insufficiency (CVI) is a long-term condition where the veins in your legs struggle to send blood back up to your heart effectively. This happens when the tiny valves inside your leg veins become damaged or weakened, allowing blood to flow backwards or pool in your lower legs.
While healthy leg veins work like a one-way system, pushing blood upwards to the heart against gravity, damaged valves can't close properly. This leads to blood pooling in your legs (known as venous reflux), causing pressure to build up inside the veins. Over time, this increased pressure can cause symptoms like swelling, aching, and skin changes.
CVI affects millions of people worldwide and usually gets worse if left untreated. The good news is that with proper diagnosis and treatment, most people can manage their symptoms effectively and prevent the condition from progressing to more serious complications like leg ulcers.
How Chronic Venous Insufficiency develops
CVI typically develops gradually when the valves in your leg veins stop working properly. These small valves are designed to encourage blood flow up your leg to the heart and to prevent blood from flowing backwards down the leg.
Valve damage can occur due to:
- Age-related wear: Valves naturally weaken over time, making them less effective
- Increased pressure: Long periods of standing or sitting can put extra strain on your leg veins
- Blood clots: Previous clots can damage valve structure permanently
- Injury or trauma: Direct damage to veins can affect how valves function
- Genetic factors: Some people are born with weaker vein walls or faulty valves
- Pregnancy: The pressure of a baby inside the uterus can put extra pressure on vein valves and cause them to fail
- Obesity: Being overweight is a risk factor for developing a number of vein problems
As blood begins to pool in your legs, the veins stretch and become enlarged. This creates a cycle where the stretched veins make it even harder for the valves to close properly, leading to more blood pooling and increased pressure. This progressive nature is why early treatment is so important.
Who is affected?
CVI can affect anyone, but certain groups face higher risks. Understanding these risk factors can help you recognise early signs and take preventive steps.
Higher risk groups include:
- Women: Pregnancy and hormonal changes increase the likelihood of developing CVI
- People over 50: Age-related changes in vein walls and valves make CVI more common
- Those with a family history: If close relatives have had vein problems, your risk may be higher
- People who stand or sit for long periods: Jobs requiring prolonged standing or desk work can strain leg veins. Examples include nurses, construction workers, teachers or office workers
- Individuals who are overweight: Extra weight puts additional pressure on leg veins
- Previous blood clot sufferers: Past clots can cause lasting damage to vein valves
The condition affects adults across the UK, with symptoms ranging from mild discomfort to severe complications. While CVI is more common in older adults, younger people can also develop it, especially if they have risk factors like pregnancy, obesity, or jobs that involve long periods of standing.
Signs and symptoms of Chronic Venous Insufficiency
CVI symptoms often develop slowly and may be mild at first, making them easy to dismiss as normal tiredness or aging. However, recognising CVI symptoms early is important for preventing the condition from worsening.

Common signs and symptoms
Physical discomfort:
- Aching or heaviness: Your legs may feel tired, especially after standing or sitting for long periods. Aching is often worse towards the end of the day
- Swelling: Usually starts around the ankles and may worsen throughout the day
- Cramping: Particularly at night or after periods of inactivity
- Restless legs: An uncomfortable feeling that makes you want to move your legs
Visible changes:
- Spider veins: Small, web-like veins visible through the skin
- Varicose veins: Enlarged, twisted veins that bulge beneath the skin
- Skin discolouration: Brown or reddish patches, usually around the ankles
When symptoms may worsen
As CVI advances, symptoms typically become more noticeable and persistent:
- Persistent swelling: May not improve with rest or elevation
- Skin changes: Thickening, hardening, brown discolouration or texture changes in the lower leg
- Itching or burning: Uncomfortable sensations in the affected areas
- Skin ulcers: Open wounds that heal slowly, usually near the ankle
These symptoms often worsen during hot weather, after long periods of standing, or at the end of the day. Many people find their symptoms improve when they elevate their legs or wear compression stockings.
Different stages of Chronic Venous Insufficiency
Medical professionals use the CEAP classification system to describe the different stages of chronic venous disease. Understanding these stages helps explain how CVI progresses and guides treatment decisions.

Early stages (C0-C2)
- C0 - No visible signs: You may have symptoms like aching or swelling, but no visible vein problems
- C1 - Spider veins: Small, fine veins visible through the skin, often considered mainly cosmetic
- C2a - Asymptomatic varicose veins: Veins that bulge beneath the skin surface, but do not cause any symptoms
Moderate stages (C3-C4)
- C2s – Symptomatic varicose veins: Larger, twisted veins that bulge beneath the skin surface and cause symptoms such as pain, aching, itching or burning
- C3 - Swelling (oedema): Noticeable swelling that may improve with rest and elevation
- C4a - Skin pigmentation: Brown or reddish discolouration, usually around the ankles
- C4c - Corona phlebectatica: Fan-shaped clusters of small veins around the ankle
Advanced stages (C5-C6)
- C4b - Skin hardening: Thickening and hardening of the skin and underlying tissue
- C5 - Healed ulcer: Previous leg ulcers that have healed but may recur
- C6 - Active ulcer: Open wounds that are slow to heal and require ongoing treatment
Most people with early-stage CVI can manage their condition effectively with lifestyle changes and conservative treatment unless they are symptomatic. However, advanced stages require more intensive medical care to prevent serious complications.
Causes and risk factors
Primary causes
CVI develops when the normal function of your leg veins becomes impaired. The most common underlying causes include:
- Valve dysfunction: When the small valves in your veins fail to close properly
- Vein wall weakness: Inherited or age-related weakening of vein structure
- Previous blood clots: Past clots can cause permanent damage to valves
- Congenital abnormalities: Some people are born with vein or valve defects
Risk factors you should know
Several factors can increase your likelihood of developing CVI, ranging from lifestyle choices you can control to medical and genetic factors that require awareness and monitoring.
Lifestyle factors:
- Prolonged standing or sitting: Jobs requiring long periods in one position
- Lack of exercise: Poor muscle tone reduces the pumping action that helps blood return to the heart
- Obesity: Extra weight increases pressure on leg veins
- Smoking: Damages blood vessels and affects circulation
Medical factors:
- Pregnancy: Increased blood volume and pressure from the growing baby
- Hormonal changes: Birth control pills, hormone replacement therapy, or menopause
- Age: Veins naturally weaken over time, typically after age 50
- Previous leg injury: Trauma that damages veins or surrounding tissue
Genetic factors:
- Family history: Having relatives with vein problems increases your risk
- Gender: Women are more likely to develop CVI due to hormonal influences
Understanding your personal risk factors can help you make informed decisions about prevention and seek early treatment when needed.
How Chronic Venous Insufficiency is diagnosed
Clinical assessment (history and examination)
Your doctor will start with a thorough examination of your legs, looking for visible signs of vein problems such as varicose veins, swelling, or skin changes. They'll also ask about your symptoms, medical history, family history, and lifestyle factors that might contribute to vein problems. They'll also conduct a quality of life assessment.
During the physical exam, your doctor may:
- Check for swelling, tenderness, or skin changes
- Feel for areas of hardened skin or tissue
- Look for signs of previous or active ulcers
- Assess the colour and texture of your skin
Diagnostic tests
Duplex ultrasound: This is the most common and reliable test for diagnosing CVI. It uses sound waves to create images of your veins and shows how blood flows through them. The test is painless and can identify which valves aren't working properly and help decide which treatment options would be best.
Additional tests may include:
- Venography: Uses contrast dye and X-rays to get detailed images of your veins
- Air or photo plethysmography: Measures how well your leg muscles pump blood back to your heart
- CT or MRI venography: Advanced imaging used in complex cases
These tests help your doctor understand the severity of your condition and plan the most appropriate treatment approach.
Treatment options for Chronic Venous Insufficiency
Treatment for CVI depends on the severity of your symptoms and the stage of your condition. Many people can manage mild to moderate CVI with conservative treatments, while others may benefit from medical procedures.
Conservative treatments
Compression therapy: Compression is often the first line of treatment for CVI, using external pressure to support your veins and improve circulation.
- Compression stockings: The foundation of CVI treatment, helping improve blood flow, reduce swelling and help improve symptoms
- Bandaging: May be used initially for severe swelling or skin changes
- Graduated compression: Provides more pressure at the ankle, gradually decreasing up the leg
Lifestyle modifications:
- Regular exercise: Walking, swimming, or cycling helps improve circulation
- Leg elevation: Raising your legs above heart level when resting
- Weight management: Maintaining a healthy weight reduces pressure on leg veins
- Avoiding prolonged standing: Taking regular breaks to move and stretch

Medical treatments
Medications:
- Venoactive drugs: Medications like diosmin or horse chestnut extract that may help reduce symptoms like pain, swelling, and heaviness. These work by strengthening vein walls and improving circulation
- Diuretics: Water tablets that help reduce fluid buildup, occasionally used for severe swelling though not typically first-line treatment as they don't address the underlying vein problem
Minimally invasive procedures: These outpatient treatments can often be done under local anaesthetic with minimal downtime. However, they’re typically used to treat superficial CVI where there may be reflux or varicose veins:
- Longer-term use of blood thinners: Particularly if you’ve had more than one clot or have a medical condition that increases your risk.
- Repeat imaging or blood tests: To check if the clot has gone and to look for any signs of damage to the veins.
- Lifestyle advice: This might include weight management, stopping smoking, and staying active to help reduce your chances of another DVT.
Preventing recurrence is a key part of your long-term care. Your healthcare team will work with you to create a plan that supports your recovery and lowers your risk of future clots.
- Sclerotherapy: A special solution is injected into problematic veins, causing them to close and fade away. Particularly effective for spider veins and smaller varicose veins
- Endovenous ablation: Uses radiofrequency heat or laser energy to seal faulty veins from the inside. The treated vein gradually dissolves as blood reroutes through healthier veins
- VenaSeal: Medical adhesive (glue) is used to close damaged veins without the need for heat. Often more comfortable as no anaesthetic injections are required along the vein
- Ambulatory phlebectomy: Surface varicose veins are removed through tiny puncture wounds that typically don't require stitches. Usually combined with other treatments for best results
What to expect during and after treatment
During your treatment
If you're diagnosed with Chronic Venous Insufficiency (CVI), treatment usually begins with conservative approaches like compression therapy and lifestyle changes. Many people start with fitted compression stockings, which you'll typically need to wear daily to see the best results.
For minimally invasive procedures, most treatments are done as outpatient procedures under local anaesthetic. You can usually return to normal activities within a few days, though you may need to avoid strenuous exercise for a week or two. Your doctor will provide specific aftercare instructions based on your treatment.
Aftercare and recovery
Recovery varies depending on your treatment approach, but most people notice gradual improvement in their symptoms over several weeks to months:
- Compression therapy: Benefits are often felt within days or weeks of consistent use
- Lifestyle changes: Improvements in symptoms typically develop over 6-12 weeks
- Medical procedures: Initial results may be visible immediately, with continued improvement over 2-6 months
You'll likely have follow-up appointments to monitor your progress and adjust treatment if needed. Many people find their quality of life improves significantly once their symptoms are well-managed.
Long-term management
CVI is a chronic condition, which means ongoing management is usually needed to maintain the benefits of treatment:
- Regular monitoring: Annual check-ups to assess your condition and adjust treatment
- Lifestyle maintenance: Keeping up with exercise, weight management, and leg elevation
- Early intervention: Promptly addressing any new symptoms or changes
With proper management, most people with CVI can prevent progression and maintain an active, comfortable lifestyle.
Preventing Chronic Venous Insufficiency
While you can't change risk factors like age or genetics, there are many steps you can take to reduce your risk of developing CVI or prevent it from worsening.
Lifestyle tips
Stay active:
- Take regular walks, even short ones throughout the day
- Use stairs instead of lifts when possible
- Try simple exercises like calf raises during long periods of sitting
Maintain healthy habits:
- Keep a healthy weight to reduce pressure on your leg veins
- Stay well hydrated to maintain good blood flow
- Avoid smoking, which damages blood vessels
Work and travel tips:
- Take regular breaks from sitting or standing
- Wear compression socks during long flights
- Stretch your legs and ankles frequently
- Consider a standing desk or ergonomic workspace setup
Early intervention
If you have risk factors for CVI, early action can make a significant difference:
- Have regular check-ups with your GP, especially if you have a family history of vein problems
- Don't ignore persistent leg symptoms like aching, swelling, or heaviness
- Consider compression stockings if you stand or sit for long periods at work
- Seek prompt treatment for any leg injuries or infections
Prevention is always better than treatment, and many of the habits that prevent CVI also improve your overall health and wellbeing.

When to seek medical advice
Signs you shouldn't ignore
Don't wait for symptoms to become severe before seeking help. Contact your GP if you experience:
- Persistent leg aching or heaviness: Especially after standing or at the end of the day
- Regular swelling: That doesn't improve with rest and elevation
- Visible vein changes: New spider veins or enlarging varicose veins
- Skin changes: Discolouration, itching, or changes in skin texture
- Night cramps: Frequent leg cramps that disturb your sleep
Urgent symptoms
Seek immediate medical attention if you develop:
- Sudden, severe leg pain and swelling: Could indicate a blood clot
- Open wounds or ulcers: Especially if they're slow to heal or show signs of infection
- Skin that feels hot to touch: May suggest infection or inflammation
- Sudden shortness of breath or chest pain: Could indicate a blood clot has travelled to your lungs
Early diagnosis and treatment of CVI can prevent progression to more serious complications and significantly improve your quality of life.
Doctors who treat this condition
Related
Varicose Veins
Post-Thrombotic Syndrome (PTS)
Venous Leg Ulcers

References
- https://www.nhs.uk/conditions/varicose-veins/ [accessed 14.07.25]
- https://www.nice.org.uk/guidance/cg168 [accessed 14.07.25]
- https://www.ncbi.nlm.nih.gov/books/NBK430975/ [accessed 14.07.25]
- https://www.ahajournals.org/doi/10.1161/circulationaha.113.006898 [accessed 14.07.25]
- https://www.ejves.com/article/S1078-5884(21)00979-5/fulltext [accessed 14.07.25]

